Ultimate CGM Guide 2026: How to Choose the Right Continuous Glucose Monitor
Continuous glucose monitors have transformed diabetes management, but with more options than ever in 2026, choosing the right CGM can feel overwhelming. Whether you have Type 1 diabetes, Type 2 diabetes, or you’re exploring metabolic health, the right CGM depends on your specific needs not marketing claims.
This guide compares FDA-cleared CGMs available in the United States, focusing on what actually matters: accuracy, wear time, calibrations, integrations, and coverage/costs costs.
Why Your CGM Choice Matters More Than You Think
Not all CGMs are created equal. While they all measure glucose in interstitial fluid (not directly in blood), they differ significantly in:
- Accuracy during critical moments (especially lows and rapid glucose changes)
- Alert reliability (relevant when you need warnings about hypoglycemia)
- Ecosystem compatibility (insulin pumps, apps and health platforms)
- Insurance coverage and out-of-pocket costs (which can vary dramatically)
- Wear time and calibration requirements (impacting daily convenience)
For people who use insulin or experience hypoglycemia, these differences aren’t just about convenience they’re about safety and effective diabetes management.
Understanding CGM Accuracy: What the Numbers Don’t Tell You
CGM readings lag behind blood glucose by approximately 5–15 minutes because they measure glucose in interstitial fluid, not blood. This lag is normal and most noticeable during rapid changes after meals, during exercise, or when treating a low.
What matters more than manufacturer specifications is real-world performance:
- How accurate is the CGM when glucose is dropping quickly?
- Does it reliably alert before dangerous lows?
- How consistent are readings during overnight hours?
- Can you trust it for insulin dosing decisions?
Safety note: If how you feel doesn’t match your CGM reading, confirm with a fingerstick and follow your healthcare provider’s guidance.
Complete CGM Comparison: Commercially Available FDA-Cleared Options in 2026
Here’s a comprehensive comparison of commercially available CGMs in the United States as of February 2026, organized around what impacts daily experience.
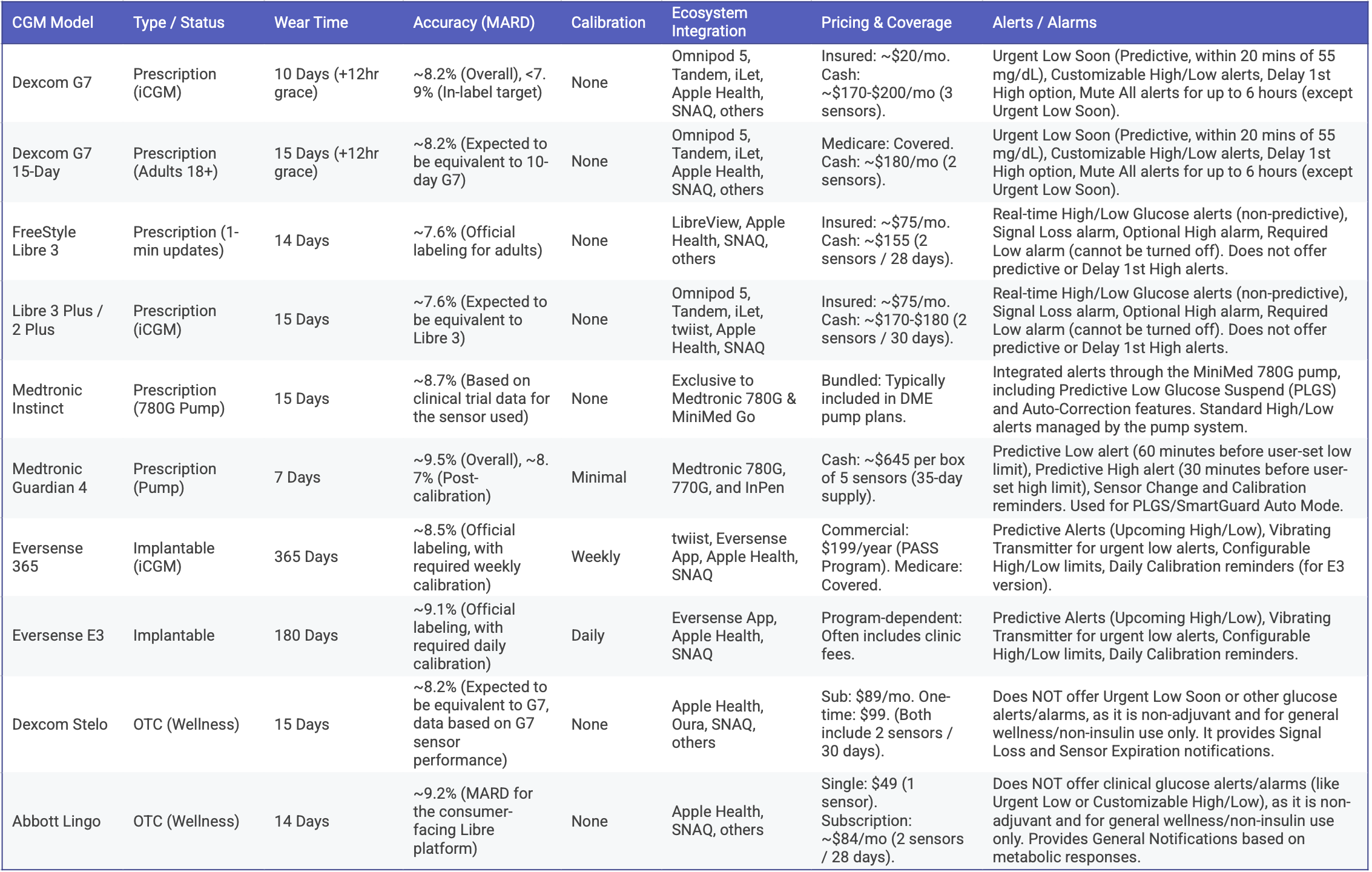
Data updated as of February 2026. Pricing and coverage vary by plan, provider and pharmacy. Check with your insurance and DME supplier for current rates.
How to Choose: Matching a CGM to Your Situation
Type 1 Diabetes
Priority: accuracy, alerts, and pump integration
Most people with Type 1 diabetes benefit from real-time CGMs with dependable low-glucose alerts. If you use an insulin pump (or plan to), ecosystem compatibility matters significantly. Dexcom G7 offers broad integration with major pump ecosystems. Medtronic users typically choose Medtronic-compatible sensors for closed-loop systems.
Accuracy during rapid changes and overnight hours is critical for safe insulin dosing. You can find more details on CGM accuracy in these articles here and here. Alarm reliability can be lifesaving, especially for those with impaired awareness of hypoglycemia.
Type 2 Diabetes on Insulin
Priority: reliable trends and affordable coverage
CGMs help reduce hypoglycemia risk and improve time-in-range. Many people find that seeing patterns not just spot checks makes decisions clearer and safer. FreeStyle Libre systems are often a strong balance of wear time and coverage for insulin users. Dexcom G7 can be especially useful if hypoglycemia is a recurring concern and you want robust alerts.
Type 2 Diabetes Without Insulin
Priority: pattern recognition and behavior change
Even without insulin, CGMs reveal how meals, timing, sleep, stress, and activity affect your glucose. The goal isn’t reacting to every spike it’s identifying repeatable patterns and making sustainable changes.
Coverage is expanding but still inconsistent, so many people pay out-of-pocket. OTC options like Dexcom Stelo or Abbott Lingo can provide prescription-free access to metabolic insights.
Pregnancy (Type 1, Insulin-Treated Type 2, or Gestational Diabetes)
Priority: tight control and clear trend visibility
Pregnancy targets are narrower than typical diabetes ranges, making consistent wear, dependable alerts, and clear trend visibility especially important. CGM use during pregnancy should always be guided by your maternal-fetal medicine team and endocrinologist.
Weight Loss and Metabolic Health
Priority: learning patterns without medical-grade alerts
OTC glucose biosensors can support food and lifestyle experimentation. Their value comes from pattern recognition across multiple days not chasing perfectly flat curves.
These sensors can help answer questions like:
- Which breakfasts keep me stable until lunch?
- Does an evening walk consistently improve overnight glucose?
- How does poor sleep affect next-day metabolism?
Insurance Coverage and Real-World Costs
Insurance coverage for CGMs varies significantly based on diagnosis, treatment plan, and the specific insurance plan:
- Medicare Part B covers CGMs for many insulin users who meet criteria (often with minimal copay)
- Commercial insurance usually covers CGMs for Type 1 diabetes and insulin-treated Type 2 diabetes
- Type 2 without insulin has expanding but inconsistent coverage (documentation may help; some plans still deny)
- OTC options (Stelo, Lingo) are typically not covered by insurance but don’t require prescriptions
Out-of-pocket costs can range from under $100/month with strong coverage to $200+ monthly for cash-pay prescription CGMs. Always verify coverage with your insurer and your preferred pharmacy/DME supplier.
Ecosystem Integration: Why It Matters
CGM data becomes more valuable when it connects with the tools you already use:
- Insulin pumps: some CGMs integrate broadly; Medtronic sensors typically pair within Medtronic-only systems
- Apple Health & Google Health: many systems now support syncing into broader health tracking
- Food and lifestyle context: apps like SNAQ can connect CGM data with meals to help identify patterns across days
Seeing glucose alongside meals, activity, sleep, and medication adds context often the missing ingredient for sustainable behavior change.
Understanding the "Why" Behind Your Glucose Data
CGMs excel at showing you what your glucose is doing in real time. But the real challenge? Understanding why it changed and what you can do differently next time.
A glucose curve on its own doesn't tell the full story. Was that spike caused by what you ate, how much you ate, or when you took your medication? Could it have been influenced by yesterday's poor sleep, today's stressful meeting, or skipping your usual walk? Without context, reacting to individual readings often leads to confusion and inconsistent decisions.
Here's what makes the difference: looking for patterns, not just data points.
Powerful insights can come from observing trends across multiple meals and days:
- Does your usual breakfast consistently lead to the same glucose response or does it vary?
- Do certain snacks cause immediate spikes, while others create delayed rises hours later?
- Does a 10-minute walk after dinner reliably flatten your curve?
Since meals are typically the strongest driver of glucose changes, understanding which foods affect you and how is one of the most impactful steps you can take.
The Bottom Line
There is no universally “best” CGM the right choice depends on your diagnosis, hypoglycemia risk, insurance coverage, and how you plan to use the data.
For Type 1 diabetes and insulin users, prioritize accuracy, alert reliability, and ecosystem integration. For Type 2 without insulin and metabolic health tracking, focus on pattern recognition and sustainable behavior change. For everyone, the best CGM is one you’ll consistently wear, trust, and understand.
Your CGM should help you make better decisions not just collect more data. Choose the system that fits your medical needs, lifestyle, and learning goals, and pair it with tools that turn glucose numbers into meaningful insights.
Ready to turn your CGM data into actionable insights? SNAQ automatically connects your glucose readings with meals, helping you discover which foods work best for your body. Learn more at www.snaq.ai.
Frequently Asked Questions
What is the most accurate CGM in 2026?
Accuracy varies by glucose range and situation. For insulin users, performance during lows and rapid changes matters most. Dexcom G7 and FreeStyle Libre 3 are both considered strong in real-world use, with Dexcom often highlighted for hypoglycemia-related alerting and experience.
Do I need a prescription for a CGM?
Most medical CGMs require prescriptions (Dexcom, Libre, Medtronic, Eversense). OTC options like Dexcom Stelo and Abbott Lingo don’t require prescriptions, but they typically aren’t covered by insurance.
Why do CGM readings differ from fingersticks?
CGMs measure glucose in interstitial fluid, which can lag blood glucose by 5–15 minutes during rapid changes. Trend arrows and direction are often more informative than single readings. Confirm with a fingerstick if symptoms don’t match the CGM.
Can I use a CGM if I don’t have diabetes?
OTC glucose biosensors (Stelo, Lingo) can be used for metabolic health and wellness without a diabetes diagnosis. Prescription CGMs typically require a diabetes-related indication.
How do I get more value from my CGM data?
Focus on patterns over multiple days rather than reacting to individual readings. Compare similar meals under similar conditions. Track food, glucose, activity and medication. Apps like SNAQ can help by automatically linking CGM data to meals so patterns become obvious and actionable.
The SNAQ website does not contain medical advice. The contents of this website, such as text, graphics, images and other material are intended for informational and educational purposes only and not for the purpose of rendering medical advice. The contents of this website are not intended to substitute for professional medical advice, diagnosis or treatment. Please consult your healthcare professional for personalized medical advice.
Questions, inputs or feedback? We are happy to hear from you at feedback@snaq.io or check out our website at snaq.io to find out more!




